Calf & Lower Leg Pain
LOWER LEG

Did you get a sudden severe pain at mid-calf, with pain on walking ever since?
If so, you may have gastrocnemius and soleus strain.
GASTROCNEMIUS AND SOLEUS STRAIN
The calf is made up of two well-known muscles, the gastrocnemius and soleus, and a little-known muscle, the plantaris. These muscles all join at the Achilles tendon.
Quick Contact
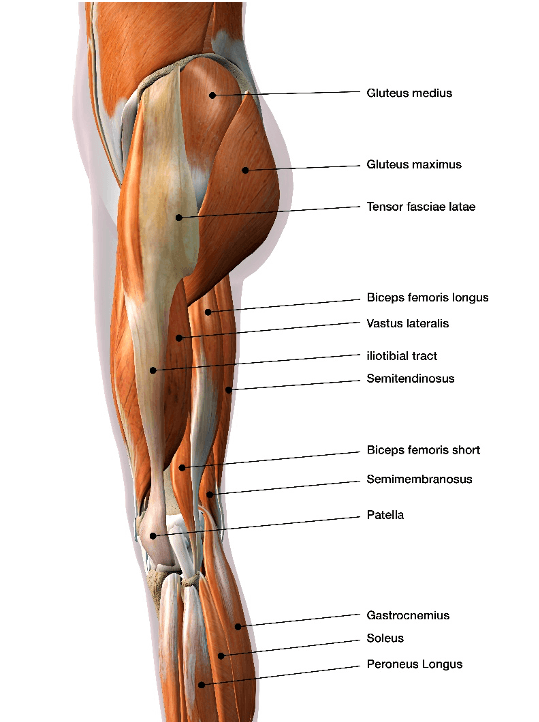 The largest muscle – the gastrocnemius – lies above the soleus and attaches above the knee joint, helping to bend the knee, whereas the soleus attaches below the knee and has no effect on the knee. Both muscles act to flex the foot down (plantarflex) through the achilles tendon. Gastrocnemius is the stronger plantar flexor when the knee is straight, with the soleus becoming stronger when the knee is bent. The gastrocnemius is more at risk of straining due to crossing two joints, and most often it is the medial head that is strained. The muscle has a high density of two fast twitch muscles, and in sport its action has been described as being like a whip.
The largest muscle – the gastrocnemius – lies above the soleus and attaches above the knee joint, helping to bend the knee, whereas the soleus attaches below the knee and has no effect on the knee. Both muscles act to flex the foot down (plantarflex) through the achilles tendon. Gastrocnemius is the stronger plantar flexor when the knee is straight, with the soleus becoming stronger when the knee is bent. The gastrocnemius is more at risk of straining due to crossing two joints, and most often it is the medial head that is strained. The muscle has a high density of two fast twitch muscles, and in sport its action has been described as being like a whip.
Soleus is considered low risk to injury – mostly slow twitch fibres – and injury tends to be slower and less traumatic than with gastrocnemius, with mild calf tightness. Walking and running can provoke discomfort that can rumble on for weeks. The plantaris also crosses the knee and ankle, it is considered vestigial, and isolated strains are difficult to identify.
A calf strain usually happens at the place where the gastrocnemius muscle joins the tendon, and starts with a sudden sharp pain. The injury is graded 1 to 3. It is possible to strain a combination of muscles, or in isolation. Physical tests – and ultimately, ultrasound scanning or MRI – give diagnostic information.
- Grade I: Twinge pain in lower leg, some aching up to five days, and you can still play sport. Initially, therapists will be careful of strong massage, and your sports injury therapist will give technology and massage as the tissue heals at appropriate stages, before progressing on to rehab in order to strengthen and stretch, helping elongate the scar tissue. Shockwave also aids with scar tissue treatment. Strength-ening starts with unloaded isometric, then isotonic and dynamic. It often takes 10 days for the tensile strength to allow this to be pain free, then you will need to do sport specific skill drills, and finally, plyometrics, i.e. hopping and jumping. Complete recovery is the goal before returning to sport. Rare complications do occur, such as myositis ossificans and compartment syndrome. Diagnosis is by physiotherapy assessment to grade and specify muscle rehab.
- Grade II: Pain on walking and initially a sharp pain in the back of the calf, bruising and some swelling, aching for a week, and pain on resisted plantar flexion (pointing toes). Treatment can include massage, electrotherapy, and specific sport physio rehab.
- Grade III: Severe pain, and you are unable to contract the muscle. There is obvious swelling and bruising. If full rupture muscle, the tear is palpable and Sever’s test positive. I have seen a handful of these.
Orthopaedic opinion and an ultrasound scan are both needed to confirm diagnosis before treatment, which can include: RICE, heel raises to ease stress on the tendon and bilateral to avoid back issues, and physiotherapy followed by shockwave, rehab massage, and stretches for grades I and II. Sport specific rehab for strengthening and balance work can also help, as well as a biomechanics check. For grade III, an orthopaedic surgical referral is always needed in case of surgery.
Did you get sudden pain on the outside of the lower leg with or without a blow? Also, does pulling your toes and foot up feel weak?
If so, you may have anterior compartment syndrome.
ANTERIOR COMPARTMENT SYNDROME
 The (front) anterior compartment space has a fascial enclosure and osseous enclosure of muscles. Anterior compartment syndrome can affect tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius, and it is potentially much more serious than shin splints. Increased pressure in the compartment can stop venous (blood) flow, which causes more swelling and pressure that can cause tissue death. The process may start with muscle swelling, then you’ll start to feel the pain. The skin may look taut and red, and the common fibular nerve may give more pain and numbness.
The (front) anterior compartment space has a fascial enclosure and osseous enclosure of muscles. Anterior compartment syndrome can affect tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius, and it is potentially much more serious than shin splints. Increased pressure in the compartment can stop venous (blood) flow, which causes more swelling and pressure that can cause tissue death. The process may start with muscle swelling, then you’ll start to feel the pain. The skin may look taut and red, and the common fibular nerve may give more pain and numbness.
For a test guideline, remember the 5 P’s: Pain, Pallor, Paraesthesia, Pulselessness, Paralysis.
This condition requires urgent medical attention, then later on, physiotherapy and a biomechanical assessment. Treatment can include: RICE, medical attention, biomechanical assessment, ultrasound, pulsed shortwave, massage, and a rehab program including exercising the upper body or cycling.
Do you get foot pain on stopping or starting from running? Do you have swelling and pain on the big toe joint? Does it hurt to pull your big toe up?
If so, you may have a metatarsophalangeal joint injury.
Do you get localised pain on the bone on the outer side of the lower leg (fibula)? Is it worse when weight bearing, especially if you have flat feet?
If so, you may have a fibula stress fracture.
FIBULA STRESS FRACTURE
This happens when either the compressive forces due to repetitive weight bearing, or the stress caused by the contraction of muscles that attach to the fibula, get too much and cause bony damage. Pain will be felt in the outer lower leg, often after running on hard ground or excessively, and in more severe cases, there may be night pain. MBST/MRT and laser can help the repair process, and rehab needs to be graded from non-weight bearing to full impact. Progression goes from cycling and swimming to water running and dynamic proprioceptive work, and finally, plyometrics.
Provisional diagnosis is by physiotherapy assessment, X-ray, biomechanical assessment, CT, and bone scan, and treatment can include: laser, orthotics, complete rest until the bone is healed, support, massage, and a gradual return to sport.
Do you get pain in an infected area? Is it sore and difficult to move the limb?
If so, you may have osteomyelitis.
OSTEOMYELITIS
This is a bone infection, and you will feel ill in addition to having a local bump over a bone with tenderness. Bacteria (staphylococcus aureus) is the most common cause of osteomyelitis, and increased risk factors include:
- Poor immune system.
- Following hip prosthesis surgery.
- Alcoholic or drug abuse.
Diagnosis is by GP for scans and bloods, and treatment options include: seeing a medic, drugs, and nutrition.
Do you get pain in the lower third of your shin bone (tibia) after running long distances, and if you press there?
If so, you may have a tibia stress fracture.
TIBIA STRESS FRACTURE
This is an incomplete crack in the shin bone. Several muscles attach to the tibia and when they contract they pull on the bone. If the loading is too excessive or repetitive, this can lead to stress fractures. A tibia stress fracture causes tenderness and pain, which tends to mostly be on the inner shin bone.
Various factors can play a role in the development of a tibia stress fracture:
- Training on too hard a surface.
- Poor foot biomechanics.
- Stiff ankle.
- Weak muscles.
- Diet lacking in minerals.
- Too obese to run.
Treatment involves soft tissue work, laser and MBST to fracture sites, Gunn IMS dry needling, guided rehab, and ankle mobs, with a biomechanics overview – especially looking for pronation – and possible orthotics with arch support.
Diagnosis is by physiotherapy assessment, and an X-ray after four weeks to show the bone is healing. Treatment can include: rest, MBST, laser, Gunn IMS, biomechanical assessment, and lower limb non-weight bearing rehab. In most cases, the individual can return to sport in eight to twelve weeks, but if more severe, this could turn into six months.
 Do you get pain on the back of your heel?
Do you get pain on the back of your heel?
Does standing on your tiptoes hurt?
If so, you may have achilles tenosynovitis.
ACHILLES TENOSYNOVITIS
Achilles tenosynovitis and achilles tendinitis usually occur together. Tendons are fibrous structures that attach muscle to bone, covered by sheaths that are lubricated by synovial fluid. Achilles tenosynovitis is also called paratenonitis, which describes the degeneration of the outer sheaf. As the tendon heals, scar tissue forms in the sheaf, attaching itself to the inner part of the tendon and causing tightness, pain, and swelling. The smooth gliding of the tendon is prevented, leading to secondary tearing. Beyond swelling and tightness, it may be possible to feel a lump at the back of the tendon.
There are multiple causes for inflammation:
- Sports activities.
- Competing triathletes.
- Systemic diseases.
- Repetitive movements.
- Poor footwear.
- Inadequate stretching.
- Hard, uneven terrain.
- Previous scar tissue.
- Sudden increase in distance.
Relative rest, cooling, and gels can help, as well as a biomechanical analysis to see if the positioning of the foot or footwear is an issue, local electrotherapy, and sport specific rehab with graded strengthening and balance work. Shockwave will soften the scar tissue, promoting healthy collagen and also promoting blood flow.
Provisional diagnosis is by physiotherapy assessment, ultrasound scan or MRI, and biomechanical assessment, and treatment can include: RICE, massage, physiotherapy, heel raises, orthotics, changing your footwear, shockwave, Gunn IMS, pulsed shortwave, ultrasound, rehab and exercises, and reduced hill running.
Do you get persistent ankle pain with swelling and locking after an ankle sprain or injury?
If so, you may have an osteochondral fracture.
OSTEOCHONDRAL FRACTURE
This is damage to the joint cartilage and underlying bone, and in the ankle this is often caused by trauma, typically from a sports injury where the shin bone is struck on the outside. Persistent ankle sprains can also lead to osteochondral fractures on the inside of the ankle.
Fragments of cartilage and bone are torn from the bone under the shin bone in the ankle (talus). If a fragment of cartilage is still attached to the bone, then conservative treatment of putting the ankle in a cast. Where fragments are only marginally attached or totally detached, then these are best removed with arthroscopic surgery.
Symptoms of osteochondral fracture include the swelling of the joint, possibly some instability, and a feeling of the joint catching with some grating.
Provisional diagnosis is by physiotherapy assessment and X-ray, and treatment can include: for grades I and II – cycling/swimming, ankle non-weight bearing exercises, laser, and a full rehab program for balance and strength. For grades III and IV – scope and surgery to remove the fragment.
Do you get a tingling or numbness in the extremities, stiff muscles or cramps, and a red rash?
If so, you may have hypocalcaemia.
HYPOCALCAEMIA
Calcium regulation is necessary for cell function – including cell membrane integrity – and ionised calcium is needed for nerve conduction, muscle relaxation, contraction, bone mineralisation, and hormones.
Diagnosis is by GP physical exam, and treatment can include: seeing a medic, and then, with their agreement, a nutritionist.
SHIN SPLINTS
These are caused by exercise, and the pain comes on after long-distance running, or sports that involve sudden turns and stops. The dull pain – which can be felt along the shin bone (tibia) – gets worse without rest. Take the pain as a warning to do activities that put less force through the tibia, then try ice, relative rest, and swimming or cycling while healing – over a couple of weeks. Once the pain is gone, make sure to run on softer ground.
It is not clear what causes microtrauma to the membrane between the bones or small fractures to the periosteum, but to reduce risk, wear good running shoes and orthotics if needed, especially if flat-footed. Run on softer ground, watch your weight, and stretch the achilles tendon before activity. A sports physio will advise you on warming up correctly, and rehab will be needed with a progressive return to your sport.
Provisional diagnosis is by physiotherapy assessment, X-ray, and biomechanical assessment, and treatment can include: orthotics, better trainers, changing your training program and using a softer surface, laser, MBST, mobilising the ankle, nutrition, and weight control. A sports therapist will take you through a graded rehab program.
Do you have unpleasant sensations in your legs, which cease on movement, and worsen in evenings?
If so, you may have restless legs syndrome.
RESTLESS LEGS SYNDROME
This affects the nervous system, and you can experience an overwhelming need to move your legs, as well as a creeping, crawling feeling in the legs. Low dopamine levels can affect this. Restless legs syndrome is occasionally linked to anaemia, kidney failure, or Parkinson’s, and it affects around one in ten people.
Diagnosis is by nutritionist, and a Gunn IMS specialist to check for lumbar spondylosis link. Treatment can include: massage, stretching, Gunn IMS, Acupuncture, reducing caffeine and alcohol, increasing your iron intake, increasing your exercise, and dopamine aiding your nutrition.
Have you had a bruising injury some months ago and do you now feel a bony lump there?
If so, you may have myositis ossificans.
MYOSITIS OSSIFICANS
This is an uncommon condition in which bone is formed inside an injured muscle. Many sports are prone to muscle injury – such as football, rugby, martial arts, and hockey – and these injuries can lead to heavy internal bleeding, evident as bruising and swelling, and can also result in a blood clot, which is an ideal breeding ground for calcification. Left untreated, the calcification can continue to develop and may take over much of the injured site over several months.
The key to prevent myositis ossificans – or the growth of bone by calcification within the injured muscle – is to seek treatment as early as possible after the injury. Once formed, the bone can only be removed surgically and the current guidelines advise waiting up to 12 months to minimise the risk of further bone growth post-surgery. The cause of myositis ossificans is not understood, and there is a risk of further bone growth post-surgery.
Diagnosis is by physiotherapy assessment, X-ray to confirm the diagnosis, and checks to confirm it is non-malignant. Treatment can include: drugs to relieve the symptoms, and surgery.
If you try to flex your foot up against resistance, does it hurt?
If so, you may have a tibialis anterior strain.
TIBIALIS ANTERIOR STRAIN
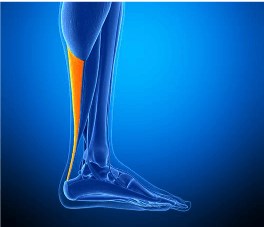
The tibialis anterior muscle runs down the outside of the shin, and when it gets sore, you feel pain at the front of the ankle. Its purpose is to lift your foot up and out. With tibialis anterior strain, the tendon can feel creaky and sore and the toes hurt to move up and down. This strain occurs when running on hard ground and is especially vulnerable with racket sports.
The provisional diagnosis is by physiotherapy assessment, and treatment can include: RICE, orthotics, shockwave, ultrasound, laser, physiotherapy, sports strengthening rehab, and proprioceptive exercise.
If you try to rotate your foot in – as if looking at the sole of your foot – against resistance, does it cause pain on the inside of your foot, but does flexing your foot up against resistance not hurt?
If so, you may have tibialis posterior tendinopathy.
TIBIALIS POSTERIOR TENDINOPATHY
The tibialis posterior originates from the back of both calf bones – the tibia and fibula – then travels down the inner side of the leg, with the tendon running behind the inner bony prominence of the ankle (medial malleolus) to attach into the foot bones. It acts to flex the foot down and rotate inwards, as when you’re trying to look at the bottom of your foot. It is also an important muscle for maintaining the arch of the foot.
A problem with tibialis posterior tendinopathy can occur either with a sudden force or repeated overuse, the latter being the more common. Symptoms of tibialis posterior tendinopathy include pain in the inner lower leg and ankle, which is made worse when running over uneven ground. Sore to touch, it can be stiff in the morning, and this can go on for weeks.
Degeneration of the tendon causes pain on the inside of the foot, and the pain is made worse if someone else tries to lift the outside of the foot (passive eversion) or if you try to press the inside of your foot down against resistance (resisted inversion). Some noise may be apparent when the tendon is activated (crepitus). In severe cases of tibialis posterior tendinopathy, the tendon can become detached and pull some of the underlying bone away (partial avulsion).
Sports prone to tibialis posterior tendinopathy include:
- Speed skaters, as they have prolonged stretching and eversion of the feet.
- Runners who develop by training around bends.
If you have flat feet or you are not fit with good balance reactions, you will be more at risk of experiencing this injury.
Diagnosis is by physiotherapy assessment, MRI or ultrasound scan to confirm, and biomechanical assessment and treatment can include: looking at your posture, orthotics to correct overpronation, physiotherapy, shockwave, laser, prescriptive proprioceptive strengthening, and rehab sports therapy to change your running program to avoid running around bends. It can take months to achieve full recovery, depending on how chronic the condition is.




