Radial shockwave provides a non-invasive gentle treatment, designed to alleviate pain and speed up recovery from injury. Despite what the name might suggest, it does not involve any kind of electrical shock treatment. Instead, it sends low energy pressure waves into damaged tissues to stimulate the body’s natural repair process, speeding up recovery and reducing inflammation.
A common concern is that treatment will be painful and the answer is reassuringly no. In fact, most clients describe the sensation as being similar to a gentle tapping on the skin.
This non-invasive treatment is very effective in treating problems such as:
- Plantar Fasciitis
- Calcified tendonitis
- Chronic tendon problems (tendinopathies)
- Achilles
- Knee
- Elbow
- Shoulder - Muscle tightness
- Legs
- Buttocks
- Spine
- Arms
We have made shockwave a standard part of the treatment we offer and have kept to our ethos of providing the best value treatment we could by providing shockwave at no extra charge. This is something we still do today and our clients love the fact that is an integral part of our hands on treatment capability.
or call 01889 881488
Committed to provide the best treatment value to you
Our clients love shockwave and we also found that they liked a device called a V-ACTOR, which is a very powerful vibrational therapy tool, the power coming from the shockwave internals. Understandably our V-ACTOR has been sought after but only having one on site has restricted access at times.
Our major focus, however, has been on the shockwave treatment and over the years as demand grew we added more shockwave machines, eventually having four.
Top Quality Treatment. Available to you at no extra cost

But our ethos remains the same – we want to provide the best treatment we can and that means the best hands on treatment, and for us that has to include both shockwave and vibrational therapy. Thus, we have taken the decision to add two more high quality shockwaves and both include the much loved V-ACTOR vibrational therapy. They are already on site and are available to you at no extra cost should you need it.
Having six shockwaves on site is perhaps a sign of our commitment to provide the best treatment value to you.
Jean, Erica & Charlotte will be happy to help
or call 01889 881488
You may have heard of gait analysis, you may even have visited your local running shop and had someone check your running out before buying the latest running shoe, but not all running gait analysis is equal and here’s why!
What if I told you that gait analysis is about more than just pronation and supination of the foot!
It's quite a bit more in fact.
or call 01889 881488
Footwear can play a big role in how your body reacts to the forces of running, but researchers have shown that some of the biggest injury risk factors are linked to your running form.
Understanding your gait for analysis
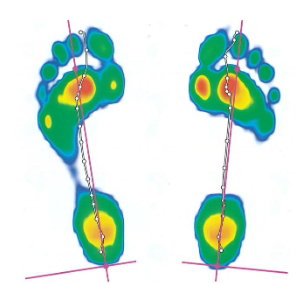
Improving your running form takes a rigorous process looking at the movements of the entire body. Our biomechanics team use `video gait analysis combined with industry leading Footscan plantar pressure data to distinguish between normal and pathological gait. This technology has been utilised in more than 3,000 scientific studies, trusted by state-of-the-art movement labs and elite sports teams worldwide.
It can also help us to make informed decisions on how best to manage your injury, be it through bespoke rehabilitation plans, running technique and coaching advice or custom orthoses.
Using Footscan we can design bespoke orthoses to aid with injury rehabilitation and performance, the same ones used by countless elite marathoners and footballers, should there be a need for them.
Aside from injury management, we also use our gait lab to help assess running technique with a view to improving running economy and performance. We can even predict overuse injury risk which is a leading cause of injuries in runners and military personnel.

From the moment you contact the ground to the moment you push off, your stride pattern speaks volumes about your injury risk and running economy, as such by analysing movement patterns and detailed data about your gait biomechanics we can really start to understand a lot more about how you could potentially move more efficiently and improve your running economy.
So, whether you are training for a marathon, or embarking on your couch to 5k this spring, we can help you solve those niggling injuries, or even unpick the lock to your next personal best!
We can help
or call 01889 881488
Tennis Elbow Part 3
Welcome back to the series of articles about physiotherapy and tennis elbow (also known as lateral epicondylitis, lateral epicondylosis and lateral epicondylalgia). So far we have covered who is affected by tennis elbow, the anatomy of the elbow and which muscles or tendons are most likely to be injured. This article will try to give an overview of a huge subject: the physiology of tendons and why they get injured, now this is a massive topic in physiotherapy and has been the subject of huge amounts of research (and in fact our knowledge on this topic is still developing) so I will only be touching the surface.
Firstly we need to look at what tendons actually are and why they might get injured in tennis elbow. Simply put a tendon is a piece of connective tissue that joins muscle to bone and is comprised of well organised mostly one directional collagen fibres (Wang et al 2003). Unlike muscles tendons can not contract themselves and are relatively inelastic (with a much lower proportion of elastin – only about 1-2% Jozsa & Kannus 1997). So basically muscles do the contraction and force generation but tendons, because they connect to the bones and are relatively inelastic, transfer that force over to the bones and move our joints. A key fact about tendons is that they generally will have a much lower blood supply than muscles and in turn have a lower metabolic rate which affects their ability to heal and makes an injury to a tendon much slower to recover and heal properly (Abate et al 2009). Furthermore the point at which muscle turns into tendon (the musculo-tendinous junction) is the point which is most often injured and is subject to large mechanical forces (Abate et al 2009).
Okay – how does this affect tennis elbow? Well, as we found out in the last article, extensor carpi radialis brevis (ECRB) is the most commonly injured muscle in tennis elbow and this muscle is most commonly injured at either the musculo-tendinous junction or at the lateral epicondyle (bony bit of the elbow) where the common extensor tendon inserts into the bone. Therefore understanding tendons and how they react and function is key to understanding tennis elbow.
The common extensor tendon as shown above is the continuation of all the extensors of the wrist and fingers and therefore any time you extend your wrist or your fingers to pick anything up it is put under stress. So it isn’t really a surprise that if you do too much of anything like picking things up then this tendon may get irritated and sore and that your physiotherapist will be able to find fairly easily a very sore spot on the lateral epicondyle of your elbow.
Next blog post will look in more detail at the physiology of what happens when the tendon gets injured in tennis elbow and hopefully manage to summarise and simplify decades of research on tendinopathies.
References
Abate M., Gravare-Silbernagel K., Siljeholm C., Di Iorio A., De Amicis D., Salini V., Werner S., Paganelli R. (2009) Pathogenesis of tendinopathies: inflammation or degeneration? Arthritis Research and Therapy 11 (3): 235
Jozsa, L., and Kannus, P., Human Tendons: Anatomy, Physiology, and Pathology. Human Kinetics: Champaign, IL, 1997
Wang J., Jia F., Yang G., Yang S., Campbell B., Stone D., Woo S., (2003) Cyclic Mechanical Stretching of Human Tendon Fibroblasts Increases the Production of Prostaglandin E2 and Levels of Cyclooxygenase Expression: A Novel In Vitro Model Study Connective Tissue Research 44: 128 – 133
Tennis Elbow Part 2
Welcome back to the new series of articles about physiotherapy and common injuries and pathologies seen by physiotherapists. Last time we took a brief look at one of the most common musculo-skeletal conditions that a physiotherapist will encounter – tennis elbow (also known as lateral epicondylitis, lateral epicondylosis and lateral epicondylalgia). This article will now look at the anatomy of the elbow and the muscles connected to it in detail so that we can have a good idea of what is hurting or being injured in tennis elbow and can maybe start to have an idea of what causes it.
Elbow Anatomy:
The elbow is an amazing piece of biomechanical design and is comprised of 3 bones – the humerus which is the upper arm bone and two bones in the forearm called the radius and ulna. The radius runs from the elbow to the thumb and the ulna starts at the bony prominence on the back of your elbow (olecranon process) and runs down to the wrist. To make it easy to remember which bone is which, when I was a student I used to repeat “the ulna is underneath the radius”. Simple I know but effective nonetheless when you are a physio student desperately trying to cram in your anatomical knowledge.
Now as we are looking at tennis elbow we are not going to look or worry too much about the actual elbow joint itself except to say that it has two ways of movement – flexion and extension (basically straightening and bending) and pronation and supination (pronation is rotating the hand palm down and supination palm up). It may seem strange that in a condition called tennis elbow we will be ignoring the elbow joint itself but hopefully the reason why will become clear soon.
The key part of the elbow in tennis elbow that we really need to examine is the lateral epicondyle – this is the point where all of the wrist extensors and finger extensors start from and is the point at which pain is felt in tennis elbow, it is also called the common extensor origin (for reasons which will become apparent soon) and is the site of attachment for the common extensor tendon. Pain here is the cardinal sign for tennis elbow that all physiotherapists look for.
Running from the lateral epicondyle and the common extensor origin are all of the muscles that extend the wrist and the fingers – extensor carpi radialis brevis, extensor carpi ulnaris, extensor digitorum, extensor indicis and extensor digiti minimi. Two other muscles have attachments at the lateral epicondyle – supinator and anconeus. All of these muscles merge together here to form what is known as the common extensor tendon which then attaches to the lateral epicondyle. So it is fairly obvious that this common extensor origin is an important point in wrist and finger extension and may well be a likely site of injury that physiotherapists will need to examine.
Before moving on it is worth considering the actions of a couple of these muscles in more detail extensor carpi radialis brevis and extensor carpi ulnaris have an important synergistic role in stabilising the wrist – they both act at the same time in concert with their flexor brothers (flexor carpi ulnaris and flexor carpi radialis) to prevent side to side movement at the wrist (ulnar and radial deviation). The two extensors also act together at the same time you grip an object to hold the wrist in extension a bit and prevent the finger flexors from flexing the wrist. In fact studies have shown that extensor carpi radialis brevis is the tendon most commonly injured in tennis elbow and the most common point that it is injured at is the common extensor tendon.
So hopefully from the above brief anatomy lesson we can now see that any extension or even flexion of the wrist is going to put a large amount of stress through the common extensor tendon and in turn if this tendon receives any injury we are likely to feel pain at the lateral epicondyle – which is where patients with tennis elbow will normally describe to their physiotherapist that they feel pain when they pick things up.
The next article will look at the physiology and some of the reasons why tendons get injured and why tennis elbow can often become chronic and last for a long time.
Tennis Elbow – Introduction
This will be the first blog post in an upcoming series about physiotherapy and common pathologies or injuries seen by physiotherapists. We will be examining in detail the causes and nature of various pathologies, who they affect, treatment options, self-management and how physiotherapy can help. The first pathology that I would like to deal with is an extremely common but frustrating and painful condition called tennis elbow that as a physiotherapist I encounter regularly in practice.
Tennis elbow has several other more complicated sounding names such as lateral epicondylitis, lateral epicondylosis and lateral epicondylalgia. All of which basically try to describe the fact that the pain people feel is at the outside (lateral) bony bit of the elbow (epicondyle). The pain normally comes on when picking up heavy objects, twisting items such as screwdrivers and can be quite sharp and uncomfortable.
It is one of the most common musculo-skeletal conditions that a physiotherapist will see and affects approximately 3 – 11/1000 patients per annum (Dingenmanse et al 2012). It is thought to occur in 1.4% of the population (Shiri et al 2006), now these do not sound like huge numbers but when you consider the size of the UK population (roughly 60 million) then 1.4% of the whole population is a lot of people! It is 7 – 9 times more common than the next most common elbow injury: golfer’s elbow (medial epicondylitis) (Walz et al 2010) and causes prolonged time off work especially in chronic sufferers (Walker-Bone et al 2012). Numerous studies have shown that it is associated with handling tools and repetitive twisting and lifting actions of the forearm (Van Rijn et al 2009) basically meaning that if you are an electrician, carpenter, manual labourer or a housewife then you are at an increased risk of developing the condition.
So… what causes it? Well that is a common question for physiotherapists and seemingly a simple question. Unfortunately it is a complicated answer and will need us to look in some detail at both the anatomy of the elbow and physiology of tendons. Which will be covered in the next blog post.
Reference List:
Dingenmanse R., Randsdorp M., Koes B., Huisstede B. (2012) Evidence for the effectiveness of electrophysical modalities for treatment of medial and lateral epicondylitis: a systematic review British Journal of Sports Medicine Published Online
Shiri R., Viikari-Juntura E., Varonen H., Heliovaara M. (2006) Prevalence and determinants of lateral and medial epicondylitis: a population study. American Journal of Epidemiology 164 (11): 1065 – 1074
Van Rijn R., Huisstede B., Koes B., Burdorf A. (2009) Associations between work-related factors and specific disorders at the elbow: a systematic literature review Rheumatology 48: 528 – 536
Walker-Bone K., Palmer K., Reading I., Coggon D., Cooper C. (2012) Occupation and epicondylitis: a population-based study. Rheumatology (Oxford) 51 (2): 305 – 310
Walz D., Newman J., Konin G., Ross G. (2010) Epicondylitis: Pathogenesis,
Imaging, and Treatment Radiographics 30 (1): 167 – 185
Injury Prevention in Tennis
Every summer, it’s time to get out your tennis shoes and racquets. It’s vital to make sure that both you and your kit are properly prepared to prevent unnecessary injury. So here are some tips and advice to help guide you:
Tennis Top Tips
- Practice hitting the ball in the “sweet spot”, the shot feels good and the impact force will be at a minimum.
- Improve your stroking technique, especially backhand
- Modern racquets do not absorb shock like the old ones. To reduce the impact on your arm:-
– Lower string tension
– Increase flexibility of racquet
– Increase racquet head size
– Add lead tape to the head to increase weight
– Increase grip size. The optimum grip circumference equals the distance from the tip of the ring finger to the crease in the middle of the palm (proximal crease)
– Grip higher up handle
– Loosen grip on handle
- Play on an appropriate surface. If you play on a hard surface the forces through the joints are much higher: twice your body weight when walking, 3 to 4 times on running and 12 times on jumping. Very dry and hard surfaces can also cause twisting ligament injuries to the knees, due to the increased friction between your shoes and the ground.
- Get a biomechanical assessment and if you need them purchase bespoke high quality orthotics. Make sure your footwear is appropriate.
- Train at an intensity lower than competitive conditions to reduce the chance of injury
- Reduce the total amount of weight bearing exercise. Do some cross training to reduce impact loading, while maintaining training volume.
- Mix training sessions with different activities. I.e. cycling, swimming.
- Set up a training diary recording rest days, sleep, heart rate and heart rate recovery time.
- If the morning your heart rate increases, decrease activity plus add in more relaxation time, and spend more time on cool down post activity.
- Eat healthily and adjust your calorie intake to activity level. Take carbs for fuel, protein for rebuilding muscle, high quality vitamin & mineral supplements and drink plenty of water.
- Enjoy the stress relief exercise can bring and don’t force yourself if you are exhausted as this is when you are most likely to get injured.
- Get regular sports massage to remove trouble spots before they become injuries.
- If in doubt see a sports physiotherapist
Warming Up and Cooling Down
Warming up is often overlooked and should be part of your injury prevention routine as there are a number of benefits:
- The muscles work better when warm and oxygenated with good blood flow.
- The joints become more flexible which reduces the pull on muscles.
- The nervous system becomes more responsive.
Including a gentle jog in your warm up will give the muscles the energy supply they need to work properly. Follow this with sport specific exercises and dynamic, sport specific stretching drills. This regime has largely replaced old fashioned static alternatives.
Examples of tennis specific exercises are running for 5 to 20 minutes with heels up to buttocks, or with high knees up to hip level. Increasing the size and speed of movements, as the body warms up and the heart rate increases, will more closely simulate competitive conditions. It is also important to focus on full body conditioning, as predominantly one sided sports, such as tennis, can cause muscle imbalances.
You should allow a total exercise and stretch time of 15 to 30 minutes and no more than 30 minutes before competing, otherwise the benefits will be lost.
Cool down should include a gentle jog plus light stretching to help eliminate waste products and reduce muscle soreness.
If you need help contact the clinic on 01889 881488 and see a physiotherapist or visit www.painreliefclinic.co.uk
Massage – Time For A New Perspective
Massage has a history which dates back thousands of years and for much of this time has been a primary medical treatment by Doctors, recognised for its ability to reduce stress, anxiety and pain, plus both help prevent and heal injuries and illnesses.
Earliest records of the use of massage in medicine were in Egypt, India and China thousands of years ago. Since then its use has expanded around the globe, with inevitable cultural variations, so we see Shiatsu from Japan, Tuina from China, Ayurveda from India and Swedish from Europe and so on.
Original concepts from India and China were to consider disease and illness as a manifestation of the body being out of balance and not in harmony with the environment. Massage was considered an important treatment to help restore balance and harmony.
In the West massage spread through Europe and was noted by Hippocrates, the Greek Physician, in 400 BC as an important part of overall health maintenance. The use of massage started to decline with the emergence of newer medical techniques and also suffered greatly due to the more unsavory euphemism for sexual services.
This very concern in fact led to the formation in the UK of the Society of Trained Masseurs, later to become the Society of Chartered Physiotherapists that we know today. Thus physiotherapy has its roots in the power of hands on healing.
In more recent years massage has had a new dawn and become available in a many forms. You can now take your pick from intensely relaxing treatments on warm water beds, to deep pressure for the less faint hearted. The basic aim remains the same: to help heal on both the physical and emotional level and enhance the overall quality of life.
Unfortunately, the true value of massage is not widely recognised in the UK and for many it is still pigeon holed as an occasional luxury, or for many men, not something they would do. But let’s go back briefly to history again. Hippocrates recognised the importance of exercise, healthy diet, rest and massage as the ingredients for maintaining or restoring health. Certainly evidence exists for example that through the ages, the Olympics have made use of this philosophy.
Now fast forward to the present day. In the 1984 Olympics, massage was listed as a medical treatment to be provided. In fact many top athletes have their own masseur. For these, diet, exercise and rest go without saying. The message is no different to that proposed by Hippocrates 2400 years ago. You can be sure massage was intensely used in the London Olympics.
In the East, massage is considered a normal medical treatment and we can look much nearer home for cultural differences to perhaps break down British prejudice. In Germany, massage is considered an important part of their preventative and treatment health care. It is quite normal for a German Doctor to prescribe a course of massage, and not drugs, for the treatment of conditions such as back pain, neck stiffness and stress.
Stress we all know is on the increase and quite simply can be a killer. The body cannot heal itself if it is continually stressed. Scientific studies have shown that excessive and uncontrolled variation in heart rate caused by stress leads to increased sickness and disease. Furthermore, just relaxing at the end of the day with your favourite tipple, cannot undo the damage caused by a full day of stress. At the clinic we measure heart rate variance (HRV) and many patients are shocked by the result. Modern technology such as HRV merely amplifies just how accurate our ancient forefathers were about health.
Time and again we see patients at our clinic, who for either physical or emotional reasons would greatly benefit from regular massage, but will not as they cannot get over the stigma of it being either a luxury or not really of therapeutic value. Without doubt, many patients would retain a more pain free existence and be less stressed, if they could overcome these barriers and adopt the attitude of many other countries.
Perhaps it is time to look again with a new perspective at massage and all it can offer you.
If you would like more information on the massage we offer or our HRV technology, then please contact the clinic on 01889 881488 or visit www.painreliefclinic.co.uk
We march into joint problems with innocent ignorance. A poor diet full of processed sugar, excess fat, caffeine and alcohol, leading to obesity, compounded by poor posture and footwear. These dark winter days we rarely get the correct amount of exercise to protect our joints, putting our bodies through repeated stresses and strains with weak muscles. On top of this it is difficult to keep a positive mindset with such negative world news.
No wonder arthritis creeps in.
My patients often ask if they have arthritis and what type. They often think that fibromyalgia is a form of arthritis.
Broadly speaking there are two kinds; osteoarthritis (OA) and rheumatoid arthritis(RA). An examination by your physiotherapist or GP with xrays and bloods, should determine which it is.
OA, the most common type, is wear and tear in the smooth cartilage protecting the bones in joints, which eventually leads to bone erosion, bone spurs and unsightly bony end thickening. The joint juice, the synovial fluid, swells and becomes inflamed and sticky. The attacked bone haemorrages precious calcium. By 50 years old 8 out of 10 of us have OA and by 60, 9 out of 10. Left untreated, OA can have a massive negative impact on quality of life and eventually need surgery. When bone is very fragile, it becomes osteoporotic and breaks easily. By the age of 70, 1 in 3 ladies suffer this.
Clearly, for everyone, it is well worth investing time to prevent the worst. I have mild OA in my right knee following surgery and if I follow the plan enclosed, I keep the symptoms at bay.
RA is totally different to OA, whereby the malfunctioning of the immune system is self destructive to joints and muscles. It is linked to genetic makeup and believed to be triggered by a viral attack.
I am frequently asked about Fibromyalgia, but this is not arthritic or inflammatory. The symptoms of fatigue, sleepless nights and muscle pain are believed to be a malfunction of the mitochondria energy processing system in the cell.
Action Plan
Exercise regulary every 48 hours, include gentle exercise like Tai Chi or Yoga when you are feeling sore and stressed up, and try to exercise outside to get your daily sunshine, vital for vitamin D.
Consult a nutritionalist to check for food allergies and consider a liver function test. Many natural products support the liver, milk thistle, artichoke and dandelion.
Increase fruit and vegetable intake, especially raw. Best for arthritis are; carrots, green peppers, watercress, tomatoes, beetroot, berries, grapes, cabbage, broccoli, brussel sprouts and kale.
Eat less red meat, dairy, sugar laden and deep fryed food, drink less alcohol and caffeinated drinks.
Increase water, ionised if possible.
Consider supplementing, check with a nutritionalist. I take high quality antioxidants, minerals and Omega 3 & 6 every day. Calcium, magnesium and phosphorus are very important for arthritis.
For fibromyalgia, 5 HTP can help sleep, try malic acid with magnesium for pain and to boost ATP energy cycle, manganese and coenzyme Q10.
Check your blood sugar level. Vitamins C,E, manganese and chromium can help with this.
Menopause can increase the problems with arthritis and fragile bones. Mineral uptake can be poorer, vitamin D low in winter, hormone levels of oestrogen and progesterone and parathyroid can be out of kilter. There are great self help books out there, and your GP can advise you on your hormones and bone density.
If pain worsens on walking, consider a biomechanical check for your footwear.
For preventive treatment ask us about on the revolutionary German MBST technology that repairs and regrows cartilage and bone cells for osteoarthritic and osteoporotic sufferers.
Suitable Therapies
For RA( rheumatoid arthritis): laser, acupuncture, physiotherapy and massage
For Fibromyalgia: the above plus Gunn IMS dry needling.
For Osteoarthritis: in addition to all the above, shockwave is excellent.
If you would like help, please contact Nicky Snazell Clinic, 01889 881488.



