Lower Back Pain Treatments
Spine problems can be complex and are often misdiagnosed. If you are suffering back pain, or one of its potential consequences such as pain in the hips, groin, knees, feet or legs, then it is vital that you choose a practice which has the capability to detect, diagnose and treat this complex condition.
Nicky Snazell Clinic has skills and technology which are unsurpassed in the UK in resolving severe and chronic lumbar spine problems.
Please click on the link to find out more about a specific condition.
QUICK CONTACT
The spine runs from the head down to the pelvis and its purpose is to provide protection for the spinal nerves, movement and shock absorption. It’s natural ‘S’ shape provides great strength to help support the body.
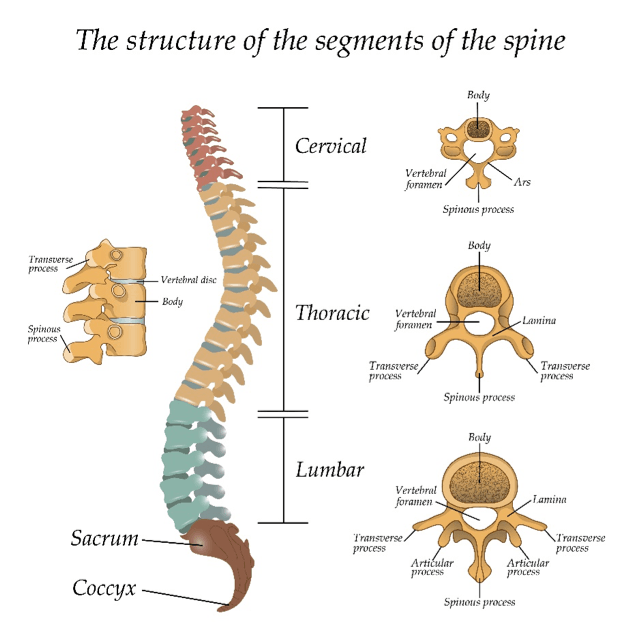
The spine is divided into 3 main sections:
- The neck, which has 7 bones, called vertebrae.
- The thoracic (rib cage), which has 12 vertebrae
- The lumbar, which has 5 vertebrae. These support the most load and are the largest vertebrae.
There is a disc between each pair of vertebrae which acts like a shock absorber. The centre of the disc is soft when younger and tends to dry out as we age. The outside of the disc is a tough annulus.
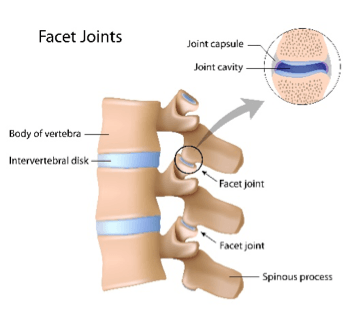
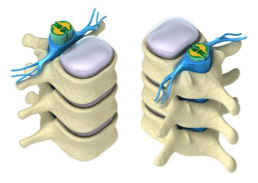
There are joints between each pair of neighbouring vertebrae, called facet joints. These joints allow for movement, such as bending or twisting and also provide added stability in the spine.
LUMBAR SPINE
The lumbar spine consists of the 5 lowest and largest vertebra and these support the highest load. The most common problem areas in the lumbar spine are associated with the 2 lowest lumbar vertebrae, called L4 and L5, but problems can also occur in L1, L2 and L3 above.
The spinal cord is linked to pairs of nerve cords which exit between each pair of vertebrae and in the lumbar are linked to the bowel, bladder, groin, hips and the legs down to the toes. Interference with these nerves can cause or be an added factor in problems in any of these areas. Examples are:
- Interference at L2 can cause problems in the groin or hips.
- Interference at L3 can cause problems in the thighs and knees
- Interference at L4 & L5 can cause problems in the lower leg and feet
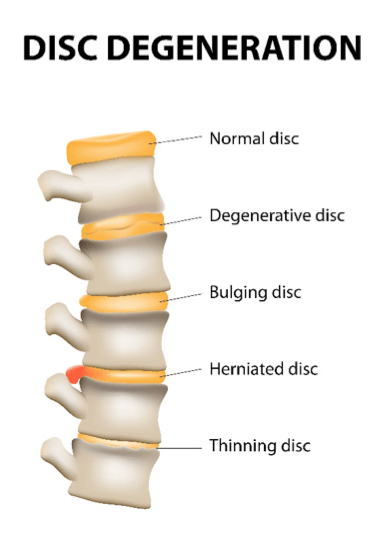 Interference with the nerves can be caused by a disc bulge or worse by a ruptured, or herniated disc. Sometimes a growth of bone can cause nerve impingement. Common symptoms can be tingling, numbness, pain, muscle tightness and after extended periods can lead to hair loss on the legs, varicose veins and toe nail problems. More serious impingements can cause loss of control of the legs, bladder or bowel.
Interference with the nerves can be caused by a disc bulge or worse by a ruptured, or herniated disc. Sometimes a growth of bone can cause nerve impingement. Common symptoms can be tingling, numbness, pain, muscle tightness and after extended periods can lead to hair loss on the legs, varicose veins and toe nail problems. More serious impingements can cause loss of control of the legs, bladder or bowel.
Additional lumbar spine problems are osteoarthritis in the facet joints, typified by stiffness in the morning or after sitting for a while and general muscle tightness causing pain and mobility issues.
Lumbar spine problems can be complex and are often misdiagnosed. MRI scans will show disc and facet joint problems, but muscle contracture is completely undetectable and as a result may lead to a patient unnecessarily suffering treatable severe and chronic pain.
If you are suffering back pain, or one of its potential consequences such as pain in the hips, groin, knees, feet or legs, then it is vital that you choose a practice which has the capability to detect, diagnose and treat the condition. Otherwise all that will happen is the symptoms rather than the cause will be treated. A sure sign of treating the symptom and not the cause is you having to keep going back for a recurring problem. If that is you now then maybe a change would be sensible.
OSTEOARTHRITIS AND FACET JOINT LOCK
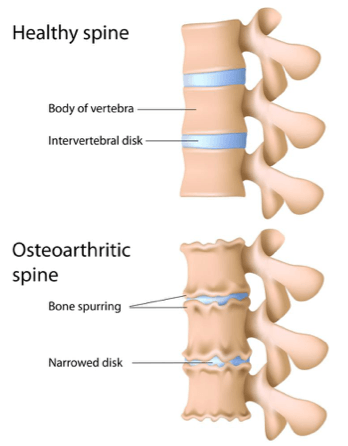 Facet joints in the lower back (lumbar) can become locked due to muscles going into spasm or a fold occurring in the joint meniscus. This can be caused by a movement or injury that has either happened recently or some time before, and movement will be restricted depending on the position the joint was locked in. To gain a range of motion, other joints near the lock will tend to be excessively moved and so pain will ensue near the lock or sometimes on the opposite side. If
Facet joints in the lower back (lumbar) can become locked due to muscles going into spasm or a fold occurring in the joint meniscus. This can be caused by a movement or injury that has either happened recently or some time before, and movement will be restricted depending on the position the joint was locked in. To gain a range of motion, other joints near the lock will tend to be excessively moved and so pain will ensue near the lock or sometimes on the opposite side. If
a facet joint in the lumbar is locked, it can cause can cause sciatica symptoms. A lack of core stability muscle control is a prime cause of lumbar facet joint lock.
Provisional diagnosis is by physiotherapy assessment, and treatment options to reduce the pain, inflammation, stiffness, and weakness include: physiotherapy, chiropractic or osteopathic mobilisations, manipulation, core stability, specific spinal rehabilitation exercises, posture advice, laser, Acupuncture, Gunn IMS dry needling, shockwave, pulsed shortwave, massage, nutrition, and counselling. MRT can be used as a preventative treatment to slow the deterioration.
Have you ever had pain suddenly occur in your back with movement, for example, when bending to tie up your laces? Is the pain localised to one spot in your back and does it not radiate out anywhere?
If so, you may have mechanical back pain
MECHANICAL BACK PAIN
Mechanical back pain is a general category that includes pain from the spinal vertebrae, joints, or soft tissues, but the source of the pain is ill-defined as usually there are no definable causes found from physical examinations or MRI scans. It can occur due to poor posture, lack of exercise, or just aging. Pain does not travel down the limbs – it remains localised – and treatment can include: manipulation, posture and exercise advice, massage, and Acupuncture.
DISC BULGE
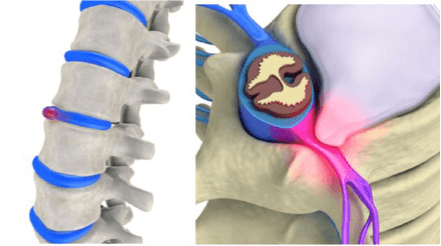 Also referred to as a slipped disc or prolapsed disc, this is when the soft disc cushion between the spinal vertebrae suffers constant loading from daily activity. Often such activities will overload the disc and cause a bulge in the side, but without the fibrous ring rupturing (becoming herniated). This is much like the bulge in a car tyre, caused by hitting a curb.
Also referred to as a slipped disc or prolapsed disc, this is when the soft disc cushion between the spinal vertebrae suffers constant loading from daily activity. Often such activities will overload the disc and cause a bulge in the side, but without the fibrous ring rupturing (becoming herniated). This is much like the bulge in a car tyre, caused by hitting a curb.
DISC PROLAPSE
A disc may bulge into the central spinal column or sideways into the exiting nerves and can, if excessive, create compression on the nerves, sufficient enough to cause local or distal pain in the limbs, numbness and weakness, and loss of motor function.
Diagnosis is by physiotherapy assessment, X-ray, and MRI, and treatment can include: Gunn IMS, electro-acupuncture, MBST, laser, and core stability rehab and exercises. If severe, surgery may be needed.
LUMBAR MUSCLE STRAINS AND LIGAMENT SPRAINS
 The lower back (lumbar) is in use for most daily activities, and is supported by strong muscles and ligaments to enable it to perform these tasks while still maintaining control. It is therefore more susceptible to injury from incorrect, excessive loading or repetitive loading; injury can occur to the muscles and connecting tendons (strain), or the ligaments (sprain), and the symptoms can be very similar. Typical symptoms include low back and buttock pain, which is aggravated by activity and which reduces with rest.
The lower back (lumbar) is in use for most daily activities, and is supported by strong muscles and ligaments to enable it to perform these tasks while still maintaining control. It is therefore more susceptible to injury from incorrect, excessive loading or repetitive loading; injury can occur to the muscles and connecting tendons (strain), or the ligaments (sprain), and the symptoms can be very similar. Typical symptoms include low back and buttock pain, which is aggravated by activity and which reduces with rest.
Lower back strains and sprains most often occur with heavy lifting – particularly when lifting and twisting – but they can also occur with sudden movement or trauma, such as during a car accident. Aggravating factors are poor core stability, obesity, and smoking, and treatment can include: Gunn IMS, physiotherapy, mobilisations, manipulation, core stability rehab and exercises, Acupuncture, shockwave, and massage.
LUMBAR SPONDYLOLYSIS
 Spondylolysis is a stress fracture in a specific area of the vertebrae called the pars interarticularis, and it most often occurs at the bottom of the lumbar spine at L5. The fracture leads to a separation of the nearby facet joints.
Spondylolysis is a stress fracture in a specific area of the vertebrae called the pars interarticularis, and it most often occurs at the bottom of the lumbar spine at L5. The fracture leads to a separation of the nearby facet joints.
Spondylolysis appears to have a hereditary link of having thinner bone structure at the pars interarticularis, which makes the probability of fracture higher. Activities where the back is repeatedly impacted while overextended (hyperextended) are prone to causing spondylolysis, and sports such as fast bowling, cricket, tennis, and gymnastics have a higher probability of repeatedly causing this condition. The problem is more common in young males, with the peak being at 16 years old.
Spondylolysis is the most common cause of spondylolisthesis, and if left untreated, spondylolysis can cause spinal stenosis, radiculopathy, and compression of the spinal cord in the lumbar region (cauda equina syndrome). Treatment can include: initially, a brace if severe, then laser, extensive core stability, one on one physiotherapy, and abstaining from aggravating activities. In severe cases, surgery may be needed.
SPONDYLOLISTHESIS
This can be either forward (anterior) or rearward (posterior) displacement of the vertebral column, and the first signs are a tightening back and hamstrings, which will lead to postural changes, the buttocks muscles (gluts) weakening, and a waddling walk. The back aches along with sciatica, causing shooting pains down the leg, from the buttock to the foot. Further symptoms can include tingling and numbness with a slipping sensation, and pain on sitting to standing. Inflammation and pain will increase with activity. If the slippage is less than 50%, the symptoms can be mild with some sciatic pain on increased activity.
The source of the pain is believed to be from tension in the centre of the inferior disc, and the nerve tunnel narrowing (foraminal stenosis) at the level of the slip. Biomechanical studies to explain the pain are found wanting. The lack of restraint on movement from the inferior facet joints adds to the stress on the disc, and slips over 50% represent only 10% of cases. Symptoms are progressive and painful, and you may also suffer from biomechanical issues, gait problems, tight hamstrings, and neurological changes (reflexes and numbness).
Posterior-only fusions tend to have more progression of their spondylolisthesis, following surgery and more pain, and degenerative changes can cause a narrowing of the spinal cord. Symptoms are the same as with spinal stenosis, neurogenic claudication, or radiculopathy, with or without back pain.
Neurogenic claudication is thought to result from central canal narrowing that is exacerbated by the listhesis (forward slip). The classic symptoms of neurogenic claudication include bilateral, posterior leg pain, which worsens with increased activity and is relieved by sitting or forward bending.
Spondylolisthesis runs in families, showing a possible genetic link. There are five types:
- Isthmic
- Degenerative
- Dysplastic
- Traumatic
- Pathologic
ISTHMIC
Isthmic spondylolisthesis (also called spondylolytic spondylolisthesis as it results from spondylolysis) is the most common form of spondylolisthesis and is a common condition. The spondylolytic defect is usually acquired between the ages of six and 16 years, and the slip often occurs shortly thereafter. Once the slip has occurred, it rarely continues to progress.
DEGENERATIVE
Degenerative spondylolisthesis is a disease of the older patients that develops as a result of facet joints getting arthritic and losing their nice chiseled shape, allowing a slip. 30 to 60% of women over 65 with osteoporosis have this problem, and these slips can go unnoticed unless there are problems with stenosis (symptoms of neurogenic claudication). This may require surgery.
DYSPLASTIC
Dysplastic spondylolisthesis is rare, and to get this you are born with damaged facet joints at the lumbar sacral junction.
TRAUMATIC
Traumatic spondylolisthesis is very rare, though it can happen in sporting accidents and may be associated with acute fracture of the inferior facets or pars interarticularis. It is currently thought that the pars interarticularis defect develops from small stress fractures that fail to heal and therefore form a chronic nonunion. There have been reports that the defect is more common among athletes who participate in sports with repeated hyperextension, such as fast bowling in cricket, gymnastics, and ballet. It is treated in the same manner as with other spinal fractures.
PATHOLOGIC
Pathologic spondylolisthesis is the last type and is also very rare. This type can occur following damage to the posterior elements from cancer secondaries or metabolic bone disease.
Treatment for these conditions can include: drugs, physiotherapy, Acupuncture, biomechanical analysis, core stability rehab, and stretches to tighten hip flexors and lumbar paraspinal muscles. If severe, seek an orthopaedic opinion, and possibly surgery.
Do you have a dull ache in the lumbar spine, both buttocks, and thighs, but not below the knees? Do you also have a dull ache after sleeping?
If so, you may have one of the following conditions: facet joint osteoarthritis or mechanical back pain (explained in the thoracic section).
Do you have any of following: burning pain, tingling, pins and needles, numbness, weakness, or coldness? Does the pain follow a line down your leg?
If so, you may have one of the following conditions:
IRRITATED SPINAL NERVES EXITING SPINAL CORD
A nerve can be compressed by a muscle contracture, disc bulge, herniation, or osteophyte growth. The pain travels down into the muscles and tissue relating to the level in the lumbar spine where it is trapped – L1, L2, etc. It can also cause digestive changes and relate to neck issues, and the pain can also track down into the groin. Problems at the lumbar 2 and 3 disc level could be mistaken for groin and hip problems, and you can feel numbness in your upper leg in the front of your thigh.
L4/5 can give you pain caused by numbness in your ankle, and if the compression is chronic, you can see hair loss in the specific skin area (dermatome).
L5/S1 can give big toe pain, and this pain will travel down the back of the leg all the way into the foot. The hamstrings at the back of the thigh can be shortened or in spasm, with the calf muscles being more at risk from injury and the plantar fascia in the sole of the foot getting tight. Numbness can be felt, or a tingling in the toes and outer aspect of the foot. Pins and needles, numbness, and pain can also occur if a peripheral nerve is affected.
A combination of problems with bladder or bowel, saddle anaesthesia (numbness around the anus), plus weakness in one or both legs, is a rare condition, resulting from a disc pressing on the spinal cord. MRI is very useful in helping to diagnose severe unrelenting pain or repeating episodes. However, bulging discs are very common and only cause a problem if the nerve is trapped.
SCIATICA
If you have sciatica, the most important treatment you can have is to get skilled and early hands-on therapy with Acupuncture – that way, you are more likely to prevent further episodes. Here is what you need to do to help the healing process during your treatment:
- Keep gently active whilst the disc is healing, and avoid activities that stir it up.
- Avoid sitting for long periods of time.
- Swap a chair for a fit ball for some of the time, and a slightly reclined, correctly aligned chair at other times.
- Drink more fluids and set new, small step goals each day.
- Get treatment and discuss this with your therapist/doctor.
- If looking at a new mattress, remember that there is no evidence to say a firm one is better. Get your back fixed before making an expensive mistake. Invest in a good mattress suitable for your weight and age. If you fear your bed is too firm, get a topper.
- If the pain is severe, see your GP for medication.
- If all else fails, a neurosurgeon may need to operate.
Diagnosis is by a pain specialist and physiotherapy assessment, and treatment can include: Gunn IMS, MBST, electro-acupuncture, physiotherapy and manipulation, laser, ultrasound, core stability, and massage.
Do you keep having spinal fractures? If so, you may have osteoporosis.
OSTEOPOROSIS
Osteoporosis is a silent disease of bone thinning that many people suffer from with no awareness whatsoever until the bones start breaking or crumbling. The pain associated with this condition can be severe and can effectively destroy any quality of life. One in three women and one in twelve men over 50 suffer osteoporosis. In the UK alone there are three million individuals with osteoporosis, and these suffer from 230,000 breaks a year.
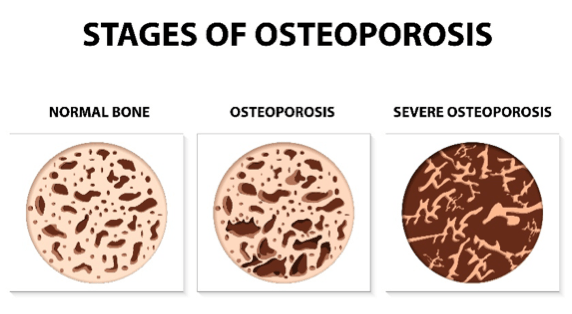
When you get a spinal fracture the pain is band-like, chronic, and over the years it gives you a hunched posture, also known as a dowager’s hump. MBST can be used to stimulate the growth of new bone, and this causes the bones to regenerate, becoming thicker and stronger and giving significant pain relief.
Treatment can include: MBST, nutritionist advice, exercise prescription, pain relief treatment such as laser with acupuncture, and meds.




